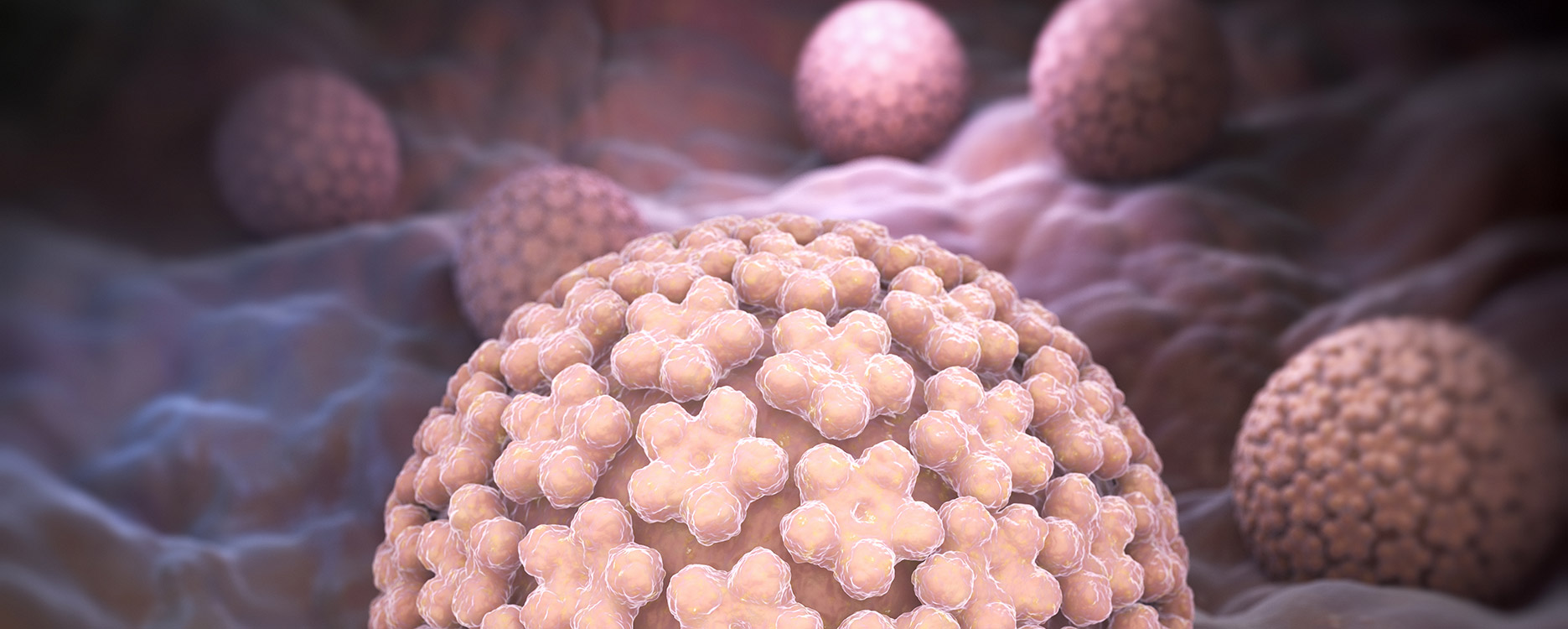
HPV, or human papillomaviruses, are widespread throughout the world. More than 100 different types of HPV are known. The majority of the population is carriers of at least one type of virus, and most often several types at the same time. Most HPVs do not manifest themselves in any way, and the person is only a carrier. Some types cause papillomas and other changes in the skin and mucous membranes. The formation of warts, laryngeal papillomas is associated with the presence of HPV, but generally these viruses are not dangerous.
The most dangerous are types of HPV, which can cause changes leading to the development of tumors. Such HPVs are called highly oncogenic. Cervical cancer is a serious cancer associated with HPV. It is characterized by a long period of precancerous changes, during which cell changes can be detected and treatment can be carried out in a timely manner.
In order to prevent the development of cervical cancer, it is very important:
Identify HPV of high oncogenic risk in a timely manner
At the same time, conduct a cytological study so as not to miss the development of pathological processes associated with HPV, including dysplasia, a precancerous condition.
It usually takes several years from the initial stage of dysplasia to the development of cancer. Early detection of HPV and dysplasia prevents cancer
Cervical cancer screening is an ideal test for regular screening.
The basis is the simultaneous conduct of liquid cytology and HPV test, which is important for a full assessment of changes.
Liquid cytology is an automated standardized technique for performing thin-layer smears that allows you to see each cell under a microscope in order to identify its changes, including oncological transformation. A mixed scraping from the cervical canal and the cervix is examined, taken with a special brush, which allows you to reach the zone of transition of the squamous epithelium of the cervix to the epithelium of the cervical canal (glandular cells). In this zone, tumor cells most often develop. Placing the obtained material in a special vial and staining according to Papanicolaou increases the quality and accuracy of the study.
HPV test includes determining:
HPV type 16 separately, as the most oncogenic (studies have shown that 1 out of 4 women with identified HPV type 16 develop cancer within several years)
HPV type 18 alone – (with carriers, cancer may develop in 1 in 9 carriers)
HPV of other highly oncogenic types (31,33,35,39,45,51,52,56,58,59,66,68) as a total result
The response is returned in the “found / not found” format. The result “detected” means that the virus has been detected in the amount that requires monitoring and / or treatment.
The fact is that HPV is a rather capricious virus. They can enter the body and spontaneously disappear with good immunity in the patient. The main routes of transmission are contact and sexual, therefore, re-infection or manifestation of the virus is possible when immunity is weakened. There are known cases when HPV is either detected or not. Usually this situation occurs with a small amount of virus and depends neither on the patient nor on the doctor. It’s all about the peculiarities of the vital activity of the virus and the process of its opposition to the immune system.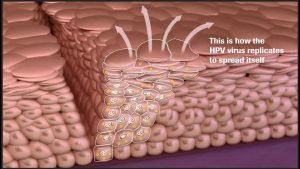
What are the advantages of cervical cancer screening compared to other tests that detect HPV?
Simultaneous cytological examination and HPV https://en.wikipedia.org/wiki/Human_papillomavirus_infection test is a strategy to identify risks as much as possible.
First, the detection of HPV in the amount that is significant allows you to plan a visit to the doctor, to be monitored and to carry out the necessary treatment, if necessary.
Secondly, cytological examination allows not to miss “suspicious” cells, if necessary, perform additional smears.
In order for the study to be as reliable as possible, it is important to properly prepare:
Do not take smears during menstruation or immediately after them, optimally – 2 days after the cessation of spotting
Before the study, exclude sexual intercourse, the use of topical drugs and douching 48 hours in advance
If a colposcopy was performed, it should take at least 2 days
Re-examination is carried out, if necessary, it is carried out – after 3 months, so that the layer of cells can fully recover.
Regular check-ups are a way to stay healthy for years to come.